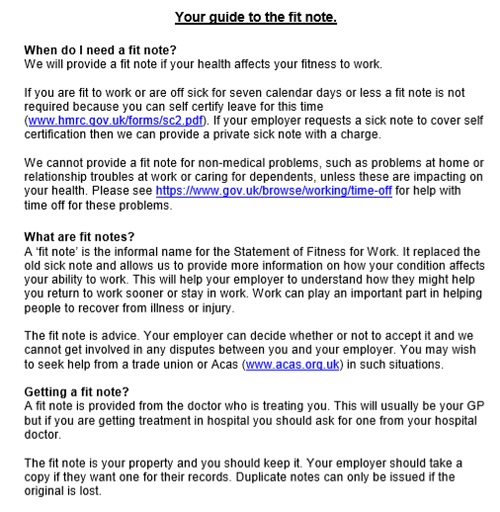
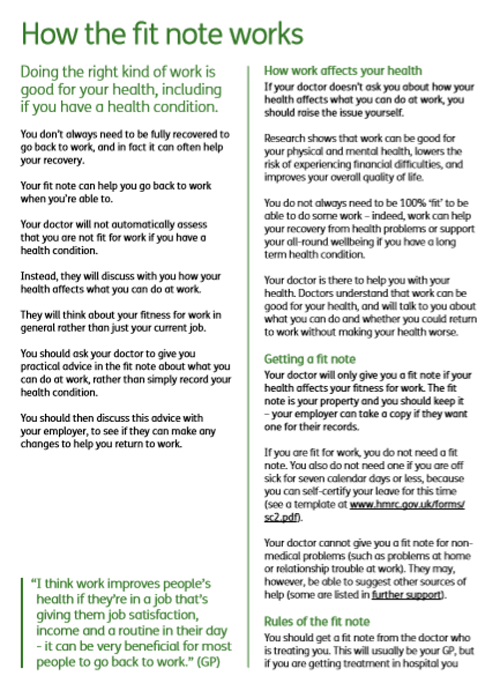
A fit note is a document written by your physician after you have been unwell for 7 days. It can be presented to your employer for two reasons. One, it can be used to certify that you are well enough to resume your duties either fully or partially. It can also show that you are unfit to go back to work at the moment. The nature of your fit note will usually depend on your doctor’s findings.
Fit notes are a record of advice. They are not legally binding on you or your employer. However, they can help clear any doubts about your condition and serve as an official record at the office.
In this article, we explain how employees and healthcare professionals can use a fit note template effectively.
Benefits of a Fit Note
A fit note may not necessarily recommend that you are completely healthy and ready to work. However, where your health might benefit from it, it might suggest that you take on lighter duties or shorter hours. In turn, your employer could arrange to support you during your recovery. They could arrange for you to have less on your plate until you are 100 percent fit.
If you work in manual labor, your fit note could suggest a gradual workload adaptation. This could help you transition into work.
Generally, your doctor will study your condition to determine what is best for you and include it in the note.
Tips for Drafting a Fit Note
A fit note template will usually include all the required fields. Nonetheless, the following tips can help ensure you get everything right. A fit note should:
- Only be drafted after someone has been away from work for more than 7 days.
- Mention specific dates and periods
- Detail exact symptoms, tests, and diagnoses
- Mention what treatment methods the doctor has applied or is recommending
- Provide recommendations to the patient’s employer
- Include the doctor’s name, title, and signature
- Include the hospital or healthcare center’s name, letterhead, and address
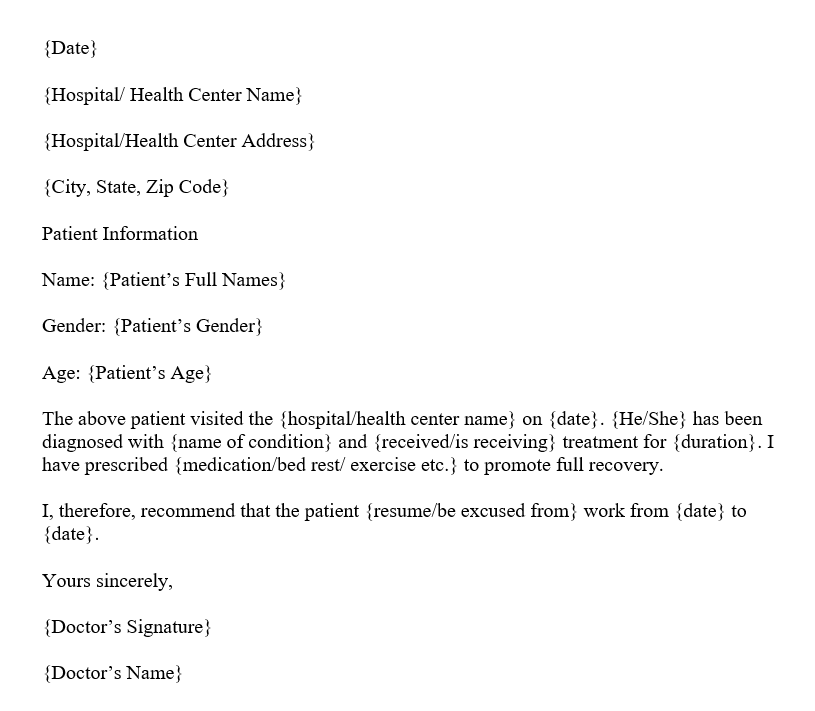
Fit Note Format
{Date}
{Hospital/ Health Center Name}
{Hospital/Health Center Address}
{City, State, Zip Code}
Patient Information
Name: {Patient’s Full Names}
Gender: {Patient’s Gender}
Age: {Patient’s Age}
The above patient visited the {hospital/health center name} on {date}. {He/She} has been diagnosed with {name of condition} and {received/is receiving} treatment for {duration}. I have prescribed {medication/bed rest/ exercise etc.} to promote full recovery.
I, therefore, recommend that the patient {resume/be excused from} work from {date} to {date}.
Yours sincerely,
{Doctor’s Signature}
{Doctor’s Name}
Sample Fit Note
18 August 2020
Sunrise Medical Center
123 Main Street
Huntington Beach, NJ 45678
Patient Information
Name: Alice Walker Jones
Gender: Female (F)
Age: 28
Ms. Alice Walker was admitted to Sunrise Medical Center on 11 August 2020. She was diagnosed with malaria and has been receiving treatment since. At the moment, it is my professional opinion that one week of bed rest will be beneficial to her health.
I, therefore, recommend that you allow Ms. Walker time off from work from 19 August 2020 to 26 August 2020.
Thank you for your consideration.
Sincerely,
Vivian Crystal, Ph.D.
Different Type of Fit Note Templates
A fit note can be handwritten by your physician. However, most hospitals have a standard fit note template that can be filled by a doctor to meet each patient’s needs. Here are a few examples:
Fit Note Template (Word Template)
- MS Word
Sample Doctor Fit Note
New Fit Note Example
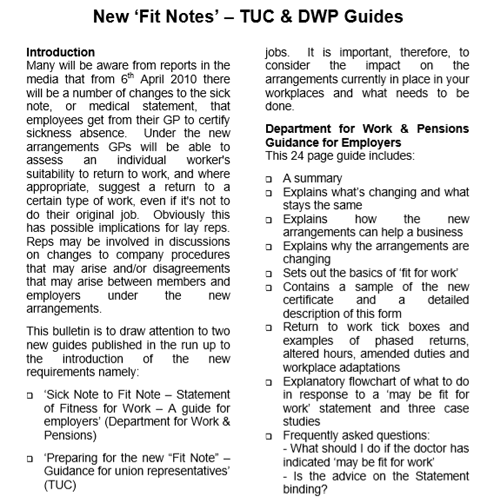
Fit for Work Note
Electronic Fit Note

Computer Fit Note
Fit Note Sample
Employer’s Fit Note
Medical Fit Note
Conclusion
After missing work for more than 7 days, a fit note can add credibility to your absence. It can help you prove you are ready to get back to work or need more time to recover. It can also encourage your employer to take suitable action concerning your situation.
Fit notes are formal documents. This means that they should be drafted professionally and accurately. To effectively achieve this, you need to use a suitable fit note template with the required fields.